Guillain-Barre Syndrome - Rehabilitation
GUILLAIN-BARRE SYNDROME – GBS (immune System Attack on Healthy Nerve Cells): Types, Causes, Symptoms & Treatment :
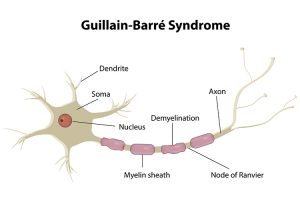
Guillain-Barre syndrome is a rare autoimmune disorder in which the immune system attacks healthy nerve cells in your peripheral nervous system. This leads to weakness, numbness, and tingling. It can eventually cause paralysis. The cause of this condition is unknown, but it’s typically triggered by an infectious illness, such as the stomach flu or a lung infection.
Types
Guillain-Barre syndrome is now known to occur in several forms.
The main types are:
- Acute inflammatory demyelinating polyradiculoneuropathy (AIDP).
- Miller Fisher syndrome (MFS)
- Acute motor axonal neuropathy (AMAN) and acute motor-sensory axonal neuropathy (AMSAN)
The first symptoms of Guillain–Barre syndrome are numbness, tingling, and pain, alone or in combination. This is followed by weakness of the legs and arms that affects both sides equally and worsens over time.
Symptoms:
- Prickling, “pins and needles” sensations in your fingers, toes, ankles or wrists
- Weakness in your legs that spreads to your upper body
- Unsteady walking or inability to walk or climb stairs
- Difficulty with eye or facial movements, including speaking, chewing or swallowing
- Severe pain that may feel achy or cramp-like and may be worse at night
- Difficulty with bladder control or bowel function
- Rapid heart rate
- Low or high blood pressure
- Difficulty breathing GBS Symptom progression: The mean time to the peak of symptoms is 12 days (from 1st neurological symptoms), with 98% of patients reaching peak by 4 weeks. A plateau phase of persistent, unchanging symptoms then ensues, followed days later by gradual symptom improvement. Recovery usually begins 2-4 weeks after the progression ceases. The mean time to clinical recovery is 200 days.
Causes:
The precise cause of Guillain-Barre is unknown. About two-thirds of people with Guillain-Barre develop it soon after they’ve been sick with diarrhea or a respiratory infection. This suggests that the disorder may be triggered by an improper immune response to the previous illness. campylobacter jejuni infection has been associated with Guillain-Barre campylobacter is one of the most common bacterial causes of diarrhea in the United States. It’s also the most common risk factor for Guillain-Barre. Campylobacter is often found in undercooked food, especially poultry.
Physiotherapy Management:
Aims of the treatment are to
- maintain clear airways
- Prevent lung infection
- Maintain anatomical joint range
- Support joint in functional position to minimize damage or deformity
- Prevention of pressure sores
- Maintain peripheral circulation
- Provide psychological support for the patient and relatives
Maintenance of clear airway & prevention of lung infection:
- Active cycle of breathing technique (ACBT) involves three phases of breathing techniques. The first phase helps you relax your airways. The second phase helps you to get air behind mucus and clears mucus. The third phase helps force the mucus out of your lungs.
- Posturally drain areas of lung tissues, 2-hourly turning into supine or side lying positions.
- A suction catheter is used to remove secretions from respective passage until the cough reflex re-appears.
- Manual techniques like vibration with/ without over pressure.
- After the removal of ventilator and adequate expansion, effective coughing must be taught to the patient
- As neurons recover, active assisted or active breathing exercises may commence with good amount of relaxing time.
To maintain normal joint movement :
Gentle passive movements through full ROM at least three times a day especially at hip , shoulder, wrist, ankle, feet.
Support joints:
Use of light splints (eg. using PLASTAZOTE) may be required for the following purpose listed below:
- Support the peripheral joints in comfortable and functional position during flaccid paralysis.
- To prevent abnormal movements.
- To stabilize patients using sandbags, pillows.
Prevention of pressure sores:
2- hourly change in patients position from supine to side lying. If the sores have developed then UVR or ice cube massage to enhance healing.
Maintenance of circulation:
- Passive movements
- Effleurage massage to lower limbs
Relief of pain:
- Transcutaneous electrical nerve stimulation
- Massage with passive ROM
- Patient can demonstrate increased sensitivity to light touch, a cradle can be used to keep the bed sheet away from the skin.
- Low pressure wrapping or snug fitting garments can provide a way to avoid light touch.
- Reassurance and explanation of what to expect can help in alleviation of anxiety that could compound the pain.
Exercises to be prescribed to the patient should be started with low repetitions and short, frequent bouts of exercises matched to the patients muscular strength. According to Bensman (1970), the following four guidelines are to be followed for prescription of exercises:
- Use short periods of non-fatiguing exercises matched to the patients strength.
- Progression of the exercise should be done only if the patient improves or if there is no deterioration in status after a week.
- Return the patient to bed rest if a decrease in muscle strength or function occurs.
- The objective should be directed towards not only at improving function but also in improving strength.
Check out these links for
relevant information: Neurological physiotherapy
For more details contact us on 📞9618906780
